Effective January 1, 2008, the Centers for Medicare and Medicaid Services (CMS) will increase its hospital outpatient reimbursement for uterine fibroid embolization (UFE) by 113 percent to $5,639 per procedure.
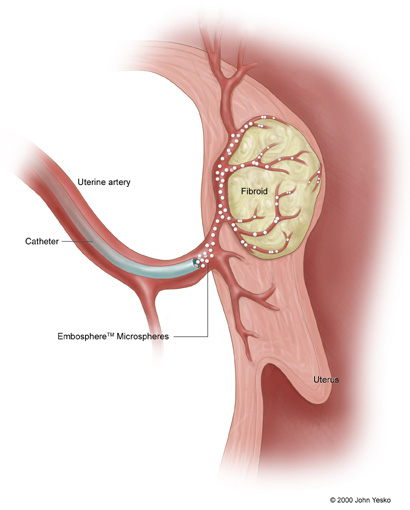 The ruling was good news for BioSphere Medical and its bioengineered microsphere technology. Microspheres, cleared by the FDA in April 2000, are injected through a catheter into the blood vessels that feed target areas – such as uterine fibroids. By selectively blocking the target tissue’s blood supply, the deprived tissue will either be destroyed or become devitalized, resulting in therapeutic benefit.
The ruling was good news for BioSphere Medical and its bioengineered microsphere technology. Microspheres, cleared by the FDA in April 2000, are injected through a catheter into the blood vessels that feed target areas – such as uterine fibroids. By selectively blocking the target tissue’s blood supply, the deprived tissue will either be destroyed or become devitalized, resulting in therapeutic benefit.
While most women seeking UFE are not Medicare beneficiaries, BioSphere believes that CMS payment decisions may influence other third-party payers. The company anticipates industry-wide adjustments that are reflective of the CMS decision. On average, the dollar amount of third-party payer payments for UFE is 33 percent greater than the dollar amount of CMS payments.
Richard Faleschini, President and Chief Executive Officer of BioSphere Medical, commented, “We believe that providers, payers, and employers also benefit from the clinical and quality-of-life advantages of UFE, and that these benefits can translate into favorable economics for all constituents. Thus, we plan to press ahead with our messaging to hospitals about the benefits of UFE, and with our ongoing strategy to have UFE included among first-line therapy options for women with symptomatic fibroids.”