OneMedRadio interviewed Alexei Marko, CEO and Director of Neovasc [CVE:NVC] where he discussed the company’s products for treating heart disease. The company’s flagship product The Reducer is in late stage development to treat refractory angina and seeks to serve a market of over 2 million patients in Europe and the United States.
Hear audio and see full transcript below.
Brett Johnson: Hi, this is Brett Johnson in New York City with OneMedRadio. Today, I’m with Alexei Marko who is the CEO of Vancouver-based Neovasc, symbol NVC on the Toronto Venture Exchange. Neovasc develops, manufactures, and markets innovative vascular devices that treat refractory angina as well as a line of other products to treat heart disease. Thanks for joining us today, Alexei.
Alexei Marko: Thank you very much, Brett.
BJ: So can you go ahead and tell us a little bit about Neovasc and your technology, its applications, and specifically the Reducer technology?
AM: We are a medical device company focused on developing products for treating heart disease. We have a number of product platforms that we’re working on. As you mentioned, the Reducer is our lead product and our flagship product that is in late stage development to treat refractory angina. Refractory angina is a debilitating late-stage heart disease that is no longer responding to other types of treatments. There is a significant patient population out there with this problem, and we are in the process of commercializing a device that we believe will address a significant number of these patients.
In addition, we also have a line of biological tissue products that we produce. That business is already at commercial stage and operating at cash flow positive, and we’re also in the early stages of developing a mitral valve replacement therapy for treating mitral valve disease.
BJ: Can you tell us a little bit about the profile of the patient? I mean who are these people and what’s their status when your technology is relevant to them?
AM: Typically, a refractory angina patient is older and has end-stage heart disease that causes significant pain upon exertion. These are patients who have typically had stents implanted previously. They may have had a bypass graft or even two, and they’re on a variety of drugs to help treat their heart disease. But we’ve reached the stage with these patients where the disease is sufficiently advanced so that there’s really not much more we can do for them. They have inadequate blood flow to certain sections of their heart, often areas that have been damaged due to having a heart attack or multiple heart attacks, and they go and see their interventional cardiologist or cardiologist with chest pain and there’s really nothing more that the physician can do for them. They may try to change their drug cocktail or try something along those lines, but essentially they’re untreatable patients with chronic heart pain that can be very debilitating.
BJ: And so what does your device do for them?
AM: Our device works in a different way than most other treatments. Most treatments focus on improving the flow of blood to the heart muscle. We acknowledge that’s a very effective approach for earlier-stage disease, but in these refractory patients, you’ve really reached the limit of what you can do with this approach. What we do instead is to work on the outflow side. So we put a little device we call the Reducer into the coronary sinus—the large vein that drains the heart muscle, and that device modulates the outflow of blood and thereby has the effect of more evenly distributing blood throughout the heart muscle. What you’ll find in these patients is there are certain territories of the heart that just aren’t getting enough blood and this is what’s causing the angina pain.
By implanting our device, what it does is essentially normalize the flow of blood through the entire heart muscle. It gets blood into these ischemic or poorly perfused areas and provides relief of these symptoms.
BJ: Interesting. Can you talk about the procedure itself and how long it takes and what’s involved?
AM: For the procedure itself, take a step back. The original idea for this was developed back in the ’50s. It was a procedure done surgically and performed largely by a US surgeon named Claude Beck, and he did this by opening the chest of the patient and going around into the coronary sinus vein on the backside of the heart and actually tying that down using a suture, thereby making it narrower.
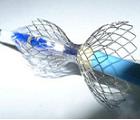
What we’ve done is come up with a contemporary way of doing this. We achieve the same positive effect that he saw doing the surgical procedure, but we do it in a procedure that takes 10 to 20 minutes using a catheter. We make a small incision in the neck. We navigate a catheter down the jugular vein into the heart, and then implant a small device. It’s very much like stent – a specialized stent with an hourglass shape. The patient is generally conscious during the procedure. It’s very quick and simple and they can be discharged the same day.
BJ: I know in one of your presentations you made it sort of akin to a garden hose and how crimping a garden hose can kind of force the blood. Is that sort of the simple way to look at this?
AM: Yes. I think that’s the best analogy that I’ve come up with to describe it. If you think about a garden hose, a leaky garden hose, if you just let the garden hose run freely, all the water will come out at the end of the garden hose and that’s really what’s happening in the case of an ischemic heart in these patients. And if you pinch off the end of the hose a little bit, you don’t stop the flow but you provide some back pressure on the outflow of the hose. You’ll find that the water will squirt out of leaks and it will also come out back of the tap where you attached the hose. Again, that’s similar to what’s happening here. You have these areas of high resistance to blood flow caused by heart disease in these patients, and the blood is avoiding them. So if you create a little bit of back pressure, what it does is essentially force blood into these areas just like you force water out of these leaks in the hose. It’s a very simple way of looking at it.
What we find is once you force blood into these areas, these sections of the heart start to contract again and start to contract more vigorously, and that further reinforces the effect, helps them open up and reduces resistance.
BJ: And this procedure you said has been effective and was done successfully many years ago.
AM: Yes, it was. As I said, it was done in the ’50s by Dr. Beck and he published a series of patient studies and he showed very good results with it. The reason it fell out of favor in the ’60s is number one, it was very invasive. It was a very difficult procedure to get into the heart and get around to these veins and suture them down as he did. Secondly, CABG or coronary artery bypass grafts became very commonplace and became a standard surgical procedure at that point in time, and they can have a very positive effect on these patients with earlier stage disease. As a result, everybody moved over to doing CABG and forgot about the Beck procedure. That doesn’t in any way diminish the underlying value of the Beck procedure, it just languished for a number of years until we started looking at it and decided that this was something that really should still be performed, but done in a much more effective, less invasive and quick way that’s in sync with contemporary medicine.
BJ: And I guess technologies have created the ability to do this thing non-invasively so that changes, you know, makes it possible. Can you tell us a where you’re at in the development of the product from a regulatory point of view?
AM: Absolutely. The product development is complete. We have done what we call our first in man study on 15 patients and we’ve actually followed those patients out to three years and the results from that study have been very, very solid. We are also in the midst of running our pivotal trial that we call COSIRA, which is enrolling between 120 and 130-patients in a double-blind, randomized, sham-controlled, multicenter study that’s being run in Europe and in Canada. We’re reaching the halfway enrollment point of that study. We expect to complete enrollment in early 2012. The endpoint for the COSIRA trial is a six-month follow-up so we expect to have all the data from the trial around the middle of 2012.
At that point, if the data are positive, we would expect to be able to get a CE mark for the Reducer, which will allow us to start selling in Europe. There is also some possibility that we might be able to get that CE mark in advance of completing the COSIRA trial. That would allow us to launch in Europe even sooner and to begin to roll-out the product there in a targeted fashion. Following completion of the COSIRA trial, we will be initiating a US trial that will be used to support an application for FDA approval and a US market launch of the product.
BJ: Can you tell us a little bit about the size of the market and how many patients are appropriate for this treatment?
AM: We would estimate that there’s about a million patients existing in Europe and about another million patients in the US who have refractory angina and are also on the patient list of cardiologists. So that will be the initial group that we can go after, and then you’re also looking at somewhere in excess of half million new patients a year coming in for treatment who would be considered refractory. If you expand that definition a little and looked at what I would call recurrent angina patients, not a true refractory case where there’s no other option, but instead who are patients receiving multiple stent implantations, they’ve had a bypass, they’re seeking continued treatments for ongoing chest pain, then there’s a significantly larger market, about a million patients a year that come into that category. So we see a very large market and a very large clinical need for the Reducer.
BJ: Any sense about the economics or what the cost of the treatment might be?
AM: The cost of the implantation is less than a typical cath lab procedure. A typical coronary stenting, I don’t know the exact procedure cost, it will depend on which center it’s performed in, typically it takes about an hour to do a routine stenting today. The procedure that we use to put our Reducer in takes significantly less than that. We are turning patients around in about 10 minutes or so. So you would expect to turn around the cath lab more rapidly than for a coronary artery stenting, which could reduce costs. The device cost itself would be very similar to a drug-eluting stent.
BJ: Terrific. And what do drug-eluting stents go for these days, for our viewers?
AM: It depends on the market, somewhere between $1000 and $2500 a unit.
BJ: All right. Okay. And then in terms of the reimbursement issues, do you see this to be easily reimbursable?
AM: Again, that depends on the jurisdiction, but I see it being easily reimbursable and it would in some cases be reimbursed under existing codes. In other cases, we would likely need to seek a new code for it.
BJ: Sure. Can you tell us a little bit about the company from a corporate point of view, sort of revenues and sort of the scope of your business, employees, and such?
AM: As I indicated, we have three product lines that we focus on. The Reducer is our flagship product. Our tissue business is at commercialization stage. We reported revenues from the tissue business of about $4.3 million in 2010 and we’re expecting to be north of $5 million in 2011. We have 50 employees and are expecting to see that grow nicely into 2012 along with revenues. As noted, we also have an early stage program that is developing a novel replacement device for mitral valve disease.
BJ: How about your background, how did you get involved in the company and what were you doing before you joined the firm?
AM: I’m an engineer by training and I’ve been working in the medical device sector for coming up on about 20 years now. I’ve been in the vascular device side of things and particularly endovascular devices for almost 15 years. I started a company in the late ’90s that developed a catheter-based product that was acquired by what eventually turned into Neovasc. I took over as the CEO of Neovasc in 2008 and in conjunction with that structured a transaction to acquire a number of companies to create the company as it is now and I have been running it for the last 3+ years .
BJ: Terrific. Well, it sounds like you have some very exciting technology and some very exciting times ahead of you.
AM: Thank you.
BJ: So thank you for joining us today. That is Alexei Marko who is the CEO of Vancouver-based Neovasc, NVC traded on the Toronto Venture Exchange. Thanks for joining us today, Alexei.
AM: You’re most welcome, Brett. I appreciate it.
BJ: This is Brett Johnson in New York City, OneMedRadio signing out. Good day.